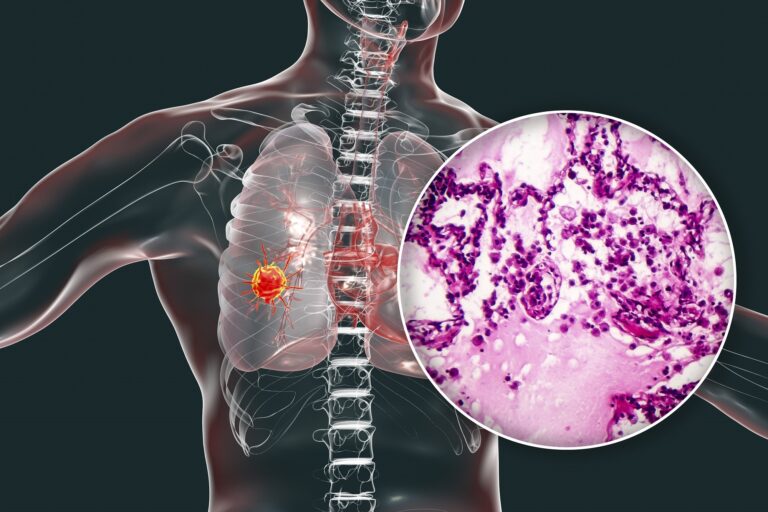
Tiny cell and non-tiny cell are the two primary kinds of cellular breakdown in the lungs. There are a few key contrasts, including the viewpoint.
In an individual with tiny cell disease, the destructive cells show up tiny and round under a magnifying instrument. The cells of non-tiny cell cellular breakdown in the lungs are bigger.
Smoking is a significant danger factor for the two kinds. Of the individuals who get a conclusion of tiny cell cellular breakdown in the lungs, 95% have a past filled with smoking.
There are a few subtypes of both tiny and non-tiny cell cellular breakdown in the lungs. Non-tiny cell cellular breakdowns in the lungs incorporate adenocarcinoma, squamous cell, and huge cell carcinoma.
Tiny cell tumors change, contingent upon the outflow of explicit qualities.
A few kinds are more forceful than others, however for the most part, tiny cell malignant growth is more forceful than non-tiny cell cellular breakdown in the lungs.
Cellular breakdown in the lungs — both tiny and non-tiny cell — is the second most regular kind of disease among grown-ups in the United States, aside from skin malignant growth. Cellular breakdown in the lungs by and large records for 14% of new malignancy analyze. Tiny cell cellular breakdown in the lungs represents 10–15% of these cases.
Manifestations
Tiny and non-tiny cell cellular breakdowns in the lungs cause comparative indications. Once in a while, side effects don’t show up until the malignancy arrives at later stages.
Manifestations include:
- a dry voice
- a steady hack
- fatigue
- shortness of breath and wheezing
- difficulty gulping
- a loss of craving
- chest torment and inconvenience
- blood in the bodily fluid raised by hacking
- swelling in the veins of the face and neck
The indications of tiny and non-tiny cell tumors are comparative, yet tiny cell malignant growth spreads all the more quickly.
An individual might be bound to encounter manifestations after cellular breakdown in the lungs has arrived at a later stage.
Causes
Causes and danger factors for tiny and non-tiny cell malignant growth will in general be comparable.
Smoking is the primary danger factor. Smoke and the synthetics that it contains can harm the lungs. This can prompt cell changes that may bring about disease.
Extra danger factors include:
- exposure to used smoke
- living in a zone with huge air contamination
- older age
- past presentation to radiation
- exposure to arsenic and different synthetic compounds
- exposure to asbestos, nickel, chromium, sediment, or tar
- having a family background of cellular breakdown in the lungs
- having HIV
Smoking is a significant danger factor for cellular breakdown in the lungs. Discover a few thoughts regarding how to stop here.
Analysis
On the off chance that an individual sees a specialist about a tenacious hack and other potential side effects of cellular breakdown in the lungs, the specialist will pose inquiries and take a clinical history. They will likewise play out a physical assessment.
In the event that cellular breakdown in the lungs might be available, the specialist will likewise demand imaging filters, for example, a X-beam or CT output, and search for indications of a tumor, scarring, or a development of liquid.
They may likewise demand tests of mucus so as to play out a sputum test. This can help demonstrate whether disease is available. The specialist will likely request that the individual give an example each morning to 3 days straight.
They may likewise play out a biopsy. This includes utilizing a needle to take an example of cells from the lungs for assessment under a magnifying instrument. They may do this during medical procedure.
A biopsy can show:
- whether cells are dangerous
- what kind of malignant growth is available, assuming any
Now and again, the specialist demands a bronchoscopy. This system includes embeddings an apparatus with an inbuilt camera through the mouth or nose and into the lungs. This encourages them see the zone and take tissue tests.
They may likewise completely differently test to decide if the disease has spread past the lungs.
Arranging
The phase of disease portrays how far it includes spread inside the body.
There are various approaches to depict the stages. One basic way is:
Restricted: This implies the disease is just in one spot.
Territorial: The disease has spread to close by tissues.
Inaccessible: The disease has spread to different pieces of the body, for instance, to the liver.
There is likewise stage 0, or “carcinoma in situ.” At this stage, there might be precancerous cells. These are not yet disease, however they may get threatening in time.
Stage 0 of cellular breakdown in the lungs implies that a specialist can’t identify dangerous cells from conventional imaging strategies, however tests have uncovered precancerous cells in the bodily fluid or somewhere else in the body.
Late stage, or metastatic, cellular breakdown in the lungs has spread to different territories of the body.
Non-tiny cell cellular breakdown in the lungs
For this kind of malignancy, specialists normally utilize a four-phase framework.
Stage 1: This implies the malignancy is just in the lungs.
Stage 2: The malignant growth has arrived at close by lymph hubs.
Stage 3: The malignant growth has spread to other lymph hubs in the chest, perhaps to those in the center or the opposite side of the chest.
Stage 4: The malignant growth has spread to the two lungs, to different pieces of the body, or both.
Phases of tiny cell cellular breakdown in the lungs
Specialists for the most part sort tiny cell cellular breakdown in the lungs with one of two phases:
The restricted stage: This implies the malignancy is on one side of the chest. It might be in one lung and, perhaps, close by lymph hubs.
The broad stage: The malignancy has spread to different pieces of the chest and different organs.
A few specialists utilize further arranging for tiny cell cellular breakdown in the lungs.
Can an individual have the two kinds?
Around 5–10% of tiny cell cellular breakdown in the lung’s cases are “blended.” This implies the individual has tiny and non-tiny cell malignant growths. Exploration proposes that it might be simpler to treat blended malignant growth than tiny cell cellular breakdown in the lungs alone.
Treatment
In the wake of making an analysis, the specialist will portray the treatment alternatives and build up a treatment plan.
Components that influence the arrangement will incorporate: – the kind of malignant growth
- how far it has spread
- the person’s age and by and large wellbeing
- the accessibility of treatments
- personal inclinations
Since every individual’s circumstance is extraordinary, treatment will change in like manner.
Non-tiny cell cellular breakdown in the lungs
Therapy choices for non-tiny cell cellular breakdown in the lungs include:
Medical procedure: A specialist will eliminate harmful cells and any close by lymph hubs that might be influenced. Notwithstanding, if disease influences an enormous part of the lungs, medical procedure may not be conceivable.
Chemotherapy: A specialist will control amazing medications that can slaughter malignant growth cells.
Endoscopic stents: If a tumor has hindered part of the aviation route, a specialist may embed a stent.
Radiation treatment: A radiologist will coordinate a light emission toward harmful cells to demolish them.
Directed therapies: These medications target explicit qualities or different variables that improve disease’s capacity to develop. Obstructing these elements can help stop or postpone the development of certain kinds of malignant growth.
Immunotherapy: This therapy expects to help the resistant framework’s capacity to protect the body against malignant growth. It is a rising treatment.
Tiny cell cellular breakdown in the lungs
For tiny cell cellular breakdown in the lungs, treatment for the most part intends to deal with the infection.
Alternatives include:
- chemotherapy, which is the primary treatment
- radiation treatment, which may help support the viability of chemotherapy or help keep the malignant growth from spreading to the cerebrum
- surgery with chemotherapy, when the disease has not yet arrived at the lymph hubs, which is uncommon
Specialists may utilize a mix of therapies for cellular breakdown in the lungs, contingent on a person’s needs, the phase of the disease, and the area of the tumor.
Standpoint
Specialists use past insights to gauge the level of individuals who are probably going to live for at least 5 years after a finding of malignancy. These assessments are called endurance rates.
They speak to midpoints and don’t consider factors, for example, an individual’s age or by and large wellbeing.
Non-tiny cell cellular breakdown in the lungs
For non-tiny cell cellular breakdown in the lungs, the American Cancer Society (ACS) report the accompanying endurance rates:
- for limited disease: 60%
- for local disease: 33%
- for far off disease: 6%
The general normal probability of living for in any event an additional 5 years is 23%.
Tiny cell cellular breakdown in the lungs
The ACS gauge the accompanying 5-year endurance rates for individuals with tiny cell cellular breakdown in the lungs:
- for confined malignancy: 29%
- for provincial malignancy: 15%
- for removed malignancy: 3%
The general normal probability of living for in any event an additional 5 years after a finding of tiny cell cellular breakdown in the lungs is 6%.
Different components that may influence endurance rates incorporate whether the disease has returned after treatment and an individual’s age. Repeating disease and progressed age can negatively affect endurance rates.
Takeaway
There are two principle sorts of cellular breakdown in the lungs: tiny cell and non-tiny cell. Tiny cell cellular breakdown in the lungs is more uncommon and more forceful.
Stopping smoking — or never smoking — can fundamentally diminish the danger of building up a cellular breakdown in the lungs.